Minimal residual disease (MRD) monitoring is a key technical method used to track residual lesions in patients after cancer treatment. It can precisely capture the small number of cancer cells, tumor-related abnormal cells, or molecular signals that may still exist after treatment, providing important evidence for doctors to more comprehensively evaluate the condition and assess the treatment effect.
"Is MRD monitoring worth doing?"
This issue has always been a concern for many cancer patients and has become one of the main worries frequently mentioned by patients during clinical communication.
Five
years ago, Mr. Ren first discovered a pulmonary nodule during a physical
examination, but no special intervention was taken. During a follow-up
examination a year ago, the nodule indicated a malignant risk, prompting him to
undergo surgical treatment and simultaneous lymph node dissection.
In July this year, in order to obtain more precise and professional postoperative treatment and follow-up guidance, Mr. Ren made a special trip to Hainan Cancer Hospital to seek diagnostic and treatment advice from Professor Yang Nong, a specially-appointed expert.
After receiving the case, Professor Yang Nong carefully studied the pathological report and imaging data and stated, "The pathological results show microinvasive lesions with partial rupture of elastic fibers, indicating that the tumor has invaded the pleura to some extent. However, this is a case of dual primary cancer, not tumor metastasis or progression, so there is no need for excessive anxiety." Based on the overall condition assessment, Professor Yang Nong provided a scientific follow-up plan - there is no need for frequent reexaminations, and a regular reexamination every six months is sufficient.

Meanwhile, Professor Yang Nong highlighted the disease risk: "Although it is currently in T1 stage (locally advanced), there is still a recurrence and metastasis probability of about 10%-20%." He suggested that Mr. Ren send the surgically removed tumor for examination, complete genetic testing, and regularly undergo MRD monitoring (tumor micro-residual disease monitoring) to timely grasp the changes in the disease and provide precise basis for subsequent diagnosis and treatment.
"Previously, some doctors suggested I undergo MRD monitoring, but Ive been hesitant. Is it really worth it?" Mr. Ren expressed his concerns and doubts.
Professor Yang Nong, drawing on his clinical experience, provided a detailed interpretation of the core value of MRD monitoring for him:
"MRD monitoring can help us accurately grasp the invisible situation in the body, and assist in understanding whether there are still trace amounts of tumor residual cells in the blood. If the monitoring results show tumor residual clearance, it indicates that the current treatment plan is effective and symptomatic, and the subsequent treatment can be carried out according to this plan; on the other hand, if there are signs of residuals, it is also convenient for timely adjustment of the diagnosis and treatment strategy. Simply put, it is like a precise navigation for the condition, which can not only assist in judging the current treatment effect, but also provide key basis for the next diagnosis and treatment decision."
To help patients better understand the significance of MRD monitoring, Professor Yang Nong further explained that MRD monitoring is not limited to a single aspect, but rather serves as a "precise tracking tool" throughout the entire process of tumor treatment:
01 For early postoperative patients, MRD monitoring can sensitively detect potential minimal tumor residuals in the blood, helping doctors predict the risk of recurrence and metastasis in advance, and then initiate intervention plans in a timely manner to reduce the probability of disease progression from the source.
02 For intermediate-stage patients who have undergone radical treatment, MRD monitoring can continuously "monitor" disease dynamics. Once signs of tumor progression are detected, it can provide a basis for adjusting treatment strategies in a timely manner, avoiding delays in the optimal diagnosis and treatment opportunities.
03 Even for patients with advanced diseases, after effective treatment, MRD monitoring can be used to assess whether the tumor burden has decreased, thereby judging the effectiveness of the current treatment and providing scientific reference for subsequent maintenance therapy or regimen optimization.
Expert Introduction / Visiting Information
【Expert Introduction】
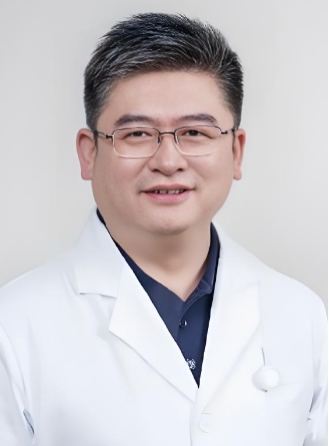
Yang Nong
Chief Physician, Doctoral Supervisor
Long-term employed experts of Hainan Cancer Hospital and Hainan Chengmei Hospital
He currently serves as Vice President of the Second Peoples Hospital of Hunan Province, leader of the oncology department, and head of the "Yang Nong Famous Doctor Clinic" / "Yang Nong Famous Doctor Expert Team Clinic". He is also the chief expert of the National Major Scientific and Technological Special Project, a member of the Lung Cancer Special Committee of the National Tumor Quality Control Center, the director of the Hunan Provincial Key Laboratory of Precision Diagnosis and Treatment of Lung Cancer, and the director of the Hunan Provincial Respiratory Tumor Clinical Medical Research Center. He has been dedicated to precision targeted therapy for lung cancer and gastrointestinal tumors, as well as to challenging recurrent and drug-resistant clinical cases, scientific research, and teaching for nearly 30 years.
He has been honored with the title of "Outstanding Model of National Famous Doctors" in the 6th session, and has been recommended as "Annual Excellent Doctor" by patients for 8 consecutive years, as well as being awarded the title of "First Brain Doctor and Famous Doctor". He has authored national guidelines, won the third prize of Hunan Provincial Science and Technology Award, garnered over 500,000 fans across the internet, and achieved over 120 million views in anti-cancer science popularization.
Medical expertise
Specialties: Precision treatment of lung cancer, breakthrough in refractory, recurrent, and drug-resistant cases with brain metastasis; individualized and precise treatment of brain metastases from lung cancer; early diagnosis of pulmonary nodules and lung cancer; personalized and comprehensive diagnosis and treatment of pan-solid tumors; clinical trials of the latest immunotherapy/targeted therapy drugs.
With nearly 30 years of experience in precision immunotherapy for lung cancer, I have led nearly 400 phase I-III clinical trials of new anticancer drugs (including national Class 1 new drugs), and am particularly skilled in treating complex cases such as refractory, recurrent, and drug-resistant conditions, as well as brain metastases.
·Early diagnosis and treatment of pulmonary nodules and lung cancer, with over 2,000 cases diagnosed annually (over 10,000 cases accumulated from 2019 to 2024), and a detection rate of over 90% (retrospective study in 2023).
·He is also proficient in the comprehensive diagnosis and treatment of multiple cancer types, individualized treatment, and interdisciplinary collaboration, covering a wide range of solid tumors (such as stomach, intestine, brain, etc.).
Professor Yang Nong has treated over 14,000 patients annually (data from 2023).
·Managed the "Lung Cancer Immunotherapy Patient Group", with long-term follow-up and management of over 4,000 lung cancer patients who have achieved long-term survival, accumulating rich clinical experience.
[Visit information]
[Clinic Hours and Location]
September 14th 8:00-12:00
Sixth Consultation Area of Hainan Cancer Hospital
[Appointment registration
Follow the official account of Hainan Cancer Hospital for "appointment registration"
[Health Consultation]
13876807106
[Friendly Reminder]
To facilitate the experts in understanding the condition as soon as possible, please bring:
1. ID card, medical insurance card, mobile phone
2. Accompany immediate family members (with decision-making authority)
3. Arrange the relevant examinations you have undergone in chronological order
4. Paper medical records of previous visits
5. Surgical case biopsy: wax block or 20-30 white slides
6. Pathological diagnosis report
7. Inpatient medical records and notes
8. Recent relevant examinations
9. The patients current treatment plan
10. The most pressing questions I want to inquire about

